Overview
People respond to stress or unfamiliar environments in many different ways. These responses, often shaped by past experiences, can be misunderstood or misinterpreted as behaviours of concern. At The Royal Children's Hospital, a key TIPC tool is the Behaviour Support Profile (BSP).
The BSP is a digital tool in the Electronic Medical Record (EMR) that documents and addresses the non-medical needs of patients, including communication preferences, sensory sensitivities, and coping strategies.
The BSP helps staff tailor care to each patient, reducing distress and enhancing their sense of safety and wellbeing. It embodies the practical application of TIPC, supporting our broader objective of transforming how we understand and respond to the needs of children and young people. Originally developed as a paper-based tool, it was integrated into the EMR in 2019. But since then, it has not yet undergone a formal evaluation.
We have evaluated the BSP's effectiveness, usability, and impact on improving hospital experiences for children, young people, families, and staff.
Our findings highlight the BSP’s potential for broader application and the need for improved accessibility, awareness, and training to maximise its benefits across the hospital.
We have developed a full and summary report of the evaluation:
Read the full BSP Evaluation Report 2025
Read the BSP Evaluation Summary 2025
Our approach
This evaluation is supported by the TIPC Working and Advisory Group, with input from the EMR team and the Centre for Health Analytics and Reporting (CHAR) for data extraction and report development.
This quality improvement project, ethically approved under the National Health and Medical Research Council (QA/9747), utilised a mixed-methods design:
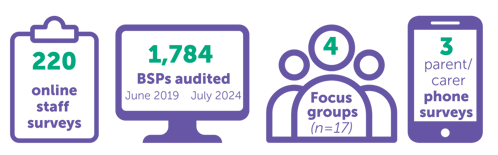
![]() Findings were analysed quantitatively and thematically to generate recommendations for optimising the BSP and improving its integration into clinical workflows. The BSP is undergoing optimisation in 2025.
Findings were analysed quantitatively and thematically to generate recommendations for optimising the BSP and improving its integration into clinical workflows. The BSP is undergoing optimisation in 2025.
Lived experience/co-design engagement
The BSP was initially developed through a co-design process involving healthcare professionals and consumer representatives. This evaluation continues to centre lived experience perspectives, ensuring that recommendations for improvement reflect the needs and priorities of the children, young people, and parents, carers and supporters.
Our team
Our team
-
Alma Giborski
-
Maddie Cranney
-
Emily Cull
-
Kelly Light
-
Dr Catherine Olweny
-
Rachel Tolan
Partners and funders
This is a Melbourne Children's Campus project that partners staff from The Royal Children's Hospital, Murdoch Children's Research Institute, and the University of Melbourne Department of Paediatrics.
The project is generously supported by The Royal Children's Hospital Foundation.
Resources
Contact us
For more information you can contact, [email protected]






