Family Centred Care
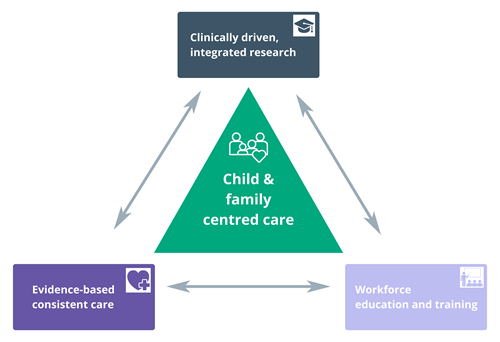
The Key Area of Family Centred Care: The objective is to design and implement an evidence-based model of family and carer (including sibling) mental health detection and support and embed this in standard care. Through research, engagement and education, this objective identifies the need to address whole child health and wellbeing through considering and supporting the environment around the child, including family and carer mental health concerns.
Acknowledgement of Country



At Mental Health Central we acknowledge the traditional custodians of the land on which we live, gather and work. We recognise their continuing connection to land, water and community. We pay respect to Elders past, present and emerging.
We acknowledge all people with a lived or living experience of mental ill-health and recovery. At the Campus, we particularly acknowledge children, young people, families, carers, and supporters. We recognise their vital contribution and value the courage of those who share this unique perspective for the purpose of learning and growing together to achieve better outcomes for the Campus, staff, sector, and all people of lived experience.